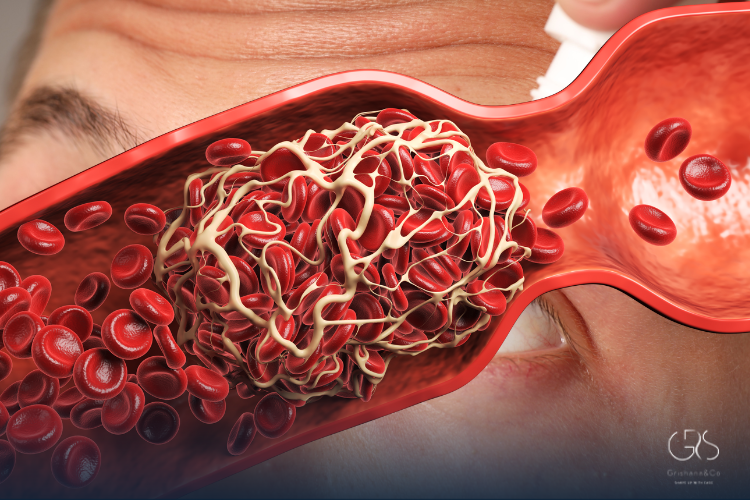
When people hear the term blood thinners, many imagine medications that literally make blood watery. In reality, these drugs do something far more specific and far more important. They reduce the blood’s ability to form dangerous clots, which can block blood flow to vital organs like the heart, lungs, or brain. Blood clots are a natural and essential part of healing, but when they form in the wrong place or at the wrong time, they can become life-threatening. This is where these medications come in. Their purpose is to lower the risk of clots that can cause heart attacks, strokes, and pulmonary embolism, while still allowing the body to stop bleeding when it truly needs to.
How Blood Thinners Work in the Body
The human body maintains a delicate balance between clotting and bleeding. Clotting involves platelets and clotting proteins working together in a cascade of reactions. Blood thinners interfere with different steps of this process. Some reduce the ability of platelets to stick together, while others block specific clotting factors produced by the liver. By interrupting these mechanisms, clot formation becomes slower and less likely to occur in blood vessels where it could cause harm. This process does not eliminate clots entirely; instead, it reduces their size and stability, making them less dangerous and easier for the body to break down naturally.
Common Types of Blood Thinners Used Today
There are several categories of these medications, each working in a slightly different way. Anticoagulants such as warfarin, apixaban, rivaroxaban, and dabigatran act on clotting proteins. Antiplatelet drugs like aspirin and clopidogrel reduce platelet aggregation. Warfarin has been used for decades and requires regular blood tests to monitor its effect, while newer direct oral anticoagulants offer more predictable dosing and fewer dietary restrictions. Doctors choose a specific option based on the patient’s condition, kidney function, age, bleeding risk, and other medications they may be taking.
When Blood Thinners Are Prescribed
Doctors prescribe these medications when the risk of harmful clotting outweighs the risk of bleeding. They are commonly recommended for people with atrial fibrillation, a heart rhythm disorder that allows blood to pool and clot in the heart. They are also used after deep vein thrombosis, pulmonary embolism, certain heart valve surgeries, and some orthopedic surgeries like hip or knee replacement. In people who have already experienced a stroke caused by a clot, these drugs can significantly reduce the risk of another event. Large clinical trials have consistently shown that appropriate use lowers mortality and serious complications in high-risk patients.
Who Might Need Blood Thinners Long-Term
Some individuals require these medications for a short period, while others may need them for life. People with mechanical heart valves almost always need lifelong therapy because artificial surfaces increase clot risk. Chronic atrial fibrillation often requires indefinite treatment as well. Genetic clotting disorders, such as factor V Leiden mutation, may also necessitate long-term use depending on personal history. The decision is always individualized and based on careful assessment of both clotting and bleeding risks.
Benefits of Blood Thinners for Heart and Brain Health
One of the most important benefits is stroke prevention. In atrial fibrillation alone, appropriate therapy can reduce stroke risk by more than 60 percent according to large meta-analyses published in major cardiology journals. These medications also prevent clots from traveling to the lungs, where they can impair oxygen exchange and strain the heart. For people with coronary artery disease, antiplatelet therapy lowers the risk of heart attack by preventing clot formation on atherosclerotic plaques. Overall, the protective effect on vital organs makes these drugs a cornerstone of modern cardiovascular care.

Risks and Side Effects You Should Know
Because they interfere with clotting, the main risk is bleeding. This can range from minor bruising or nosebleeds to more serious internal bleeding. Gastrointestinal bleeding and brain hemorrhage are rare but serious complications. The risk depends on dosage, age, kidney function, alcohol intake, and interactions with other drugs. Studies show that while bleeding risk exists, the net clinical benefit remains strongly positive for patients with clear indications. Regular follow-up and dose adjustments are key to minimizing harm.
How Blood Thinners Interact With Food and Medications
Certain foods and medications can affect how these drugs work. Warfarin, in particular, is influenced by vitamin K intake, which is found in leafy green vegetables. This does not mean patients must avoid these foods, but consistency is crucial. Many antibiotics, antifungals, and herbal supplements can increase or decrease drug levels. Newer agents have fewer interactions, but it is still essential to inform healthcare providers about all medications and supplements being used.
How Doctors Monitor Blood Thinner Therapy
Monitoring depends on the specific drug. Warfarin requires regular INR blood tests to ensure the dose is effective but safe. Direct oral anticoagulants usually do not need routine blood testing, but kidney function should be checked periodically. Doctors also monitor for signs of bleeding, anemia, or clot recurrence. Patient education plays a major role, as recognizing early warning signs can prevent serious complications.
Living Safely While Taking Blood Thinners
Daily life does not have to stop, but some precautions are wise. Using a soft toothbrush, electric razor, and avoiding high-risk activities can reduce injury-related bleeding. Wearing medical alert identification helps emergency providers respond appropriately. Patients are encouraged to maintain open communication with their healthcare team and never stop medication abruptly without medical advice, as sudden discontinuation can dramatically increase clot risk.
Special Situations: Surgery, Pregnancy, and Travel
Before surgery or dental procedures, temporary interruption may be necessary, sometimes with alternative short-acting medications. Pregnancy requires special consideration because some drugs cross the placenta and can harm the fetus. Long flights increase clot risk, and therapy may be particularly protective in these situations. Each scenario requires individualized planning guided by evidence-based protocols.
Blood Thinners and Scientific Evidence
Decades of research support the use of these medications. Landmark trials such as the RE-LY, ARISTOTLE, and ROCKET AF studies demonstrated that newer agents are at least as effective as warfarin, with similar or lower bleeding risk in many patients. Systematic reviews published in journals like The Lancet and Circulation confirm their role in preventing stroke, venous thromboembolism, and cardiovascular death across diverse populations.
Conclusion
Blood thinners play a critical role in preventing life-threatening clots and protecting the heart, brain, and lungs. While they carry risks, decades of high-quality scientific evidence show that for the right patient, the benefits far outweigh the dangers. Understanding how these medications work, why they are prescribed, and how to use them safely empowers patients to take an active role in their health. With proper monitoring and communication with healthcare providers, they remain one of the most effective tools in modern medicine.