Blood clots, medically known as thrombosis, are a leading cause of morbidity and mortality worldwide. They can obstruct the normal flow of blood in veins or arteries, resulting in life-threatening complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), heart attack, or stroke. Understanding how to prevent blood clots is therefore essential not only for high-risk individuals but for the general population seeking to preserve vascular health.
According to the Centers for Disease Control and Prevention (CDC), blood clots affect nearly 900,000 Americans annually, with approximately 100,000 deaths attributed to DVT and PE combined. Many of these cases are preventable with lifestyle modifications, timely medical attention, and awareness of the contributing risk factors.
This article presents a comprehensive, evidence-based review of how to prevent blood clots, including lifestyle interventions, clinical measures, and medication guidance, supported by recent scientific research.
Understanding Blood Clots (Thrombosis Basics)
A blood clot forms when blood changes from a liquid to a semi-solid or gel-like state. Normally, clotting (coagulation) is a protective mechanism that prevents excessive bleeding when a blood vessel is injured. However, pathological clot formation within intact vessels can lead to thrombosis, causing partial or complete blockage of blood flow.
The process of abnormal clot formation is explained by Virchow’s triad, which includes three primary contributors:
Venous stasis – slow or reduced blood flow, often caused by immobility or sedentary lifestyle.
Endothelial injury – damage to the inner lining of blood vessels due to surgery, trauma, or inflammation.
Hypercoagulability – an increased tendency of blood to clot, which may be genetic or acquired through conditions like cancer, pregnancy, or certain medications.
Understanding these mechanisms provides a scientific foundation for developing preventive measures and highlights why learning how to prevent blood clots is vital to long-term vascular health.
Risk Factors for Blood Clots
Several factors can increase the risk of thrombosis. These can be classified as inherited (genetic) or acquired:
Genetic (Inherited) Factors
Factor V Leiden mutation – the most common inherited cause of thrombophilia.
Prothrombin gene mutation (G20210A).
Protein C, Protein S, or Antithrombin III deficiency, which affect the body’s natural anticoagulant mechanisms.
Acquired Risk Factors
Prolonged immobility – during long flights, bed rest, or hospitalization.
Obesity – increases venous pressure and inflammation.
Smoking – damages vascular endothelium and promotes clot formation.
Surgery or trauma – particularly orthopedic and abdominal procedures.
Pregnancy and postpartum period – due to hormonal and circulatory changes.
Hormone therapy or oral contraceptives – may increase coagulability.
Cancer – malignancy and chemotherapy are strongly associated with thrombosis.
Infections (including COVID-19) – can trigger inflammatory pathways leading to clotting.
Awareness of these risk factors is the first step toward learning how to prevent blood clots effectively.
How to Prevent Blood Clots through Lifestyle and Habits
Lifestyle interventions are the cornerstone of clot prevention. Scientific evidence consistently supports the role of physical activity, hydration, nutrition, and avoidance of harmful substances in reducing thrombosis risk.
1. Regular Physical Activity
Physical inactivity contributes significantly to venous stasis. The World Health Organization (WHO) recommends at least 150 minutes of moderate aerobic activity per week. Walking, cycling, and swimming improve circulation and strengthen calf muscles, which assist in venous return.(I recommend that you read about the health benefits of walking)
Even small movements—such as flexing ankles, rotating legs, or standing every hour during long work sessions—can dramatically lower the risk of DVT. This is one of the simplest yet most effective ways to prevent blood clots in daily life.

2. Maintain Adequate Hydration
Dehydration thickens the blood and promotes clot formation. Adults should aim for 2–3 liters of fluids per day, primarily from water and unsweetened beverages. Hydration is especially crucial during travel, hot weather, and illness.
3. Healthy Diet and Weight Management
A balanced diet rich in fruits, vegetables, lean proteins, and omega-3 fatty acids helps reduce inflammation and maintain vascular elasticity. Foods like salmon, walnuts, and flaxseeds support endothelial health. Limiting sodium intake and avoiding processed foods can reduce hypertension—a known risk factor for vascular damage.
Maintaining a healthy body mass index (BMI) under 25 significantly lowers the risk of thrombosis and improves overall cardiovascular function.
4. Avoid Smoking and Limit Alcohol
Nicotine and tobacco toxins injure the endothelial lining, making platelets stickier and more likely to form clots. Complete cessation is essential for those seeking how to prevent blood clots and maintain vascular integrity.
Moderate alcohol intake (1 drink per day for women, 2 for men) may have neutral effects, but excessive use increases clotting risk and should be avoided.
How to Prevent Blood Clots during Travel and Hospitalization
Extended immobility—such as during long flights or hospital stays—is a well-documented risk factor for venous thrombosis.
1. During Air Travel
Move every 1–2 hours: walk the aisle or perform seated leg exercises.
Wear graduated compression stockings: evidence shows they significantly reduce DVT risk during flights longer than four hours.
Stay hydrated: avoid excessive caffeine and alcohol.
Choose an aisle seat to facilitate movement.
2. During Hospitalization or Bed Rest
Early ambulation: getting up and walking soon after surgery is a key component of postoperative thrombosis prevention.
Sequential compression devices (SCDs): used in hospitals to promote venous blood flow.
Leg elevation and gentle range-of-motion exercises: improve circulation and reduce stasis.
These practical steps are clinically proven ways to prevent blood clots in both inpatient and outpatient settings.
Medical Strategies: Medications and Monitoring
For individuals at high risk—such as those recovering from surgery, living with atrial fibrillation, or having a history of thrombosis—medical prevention plays a critical role.
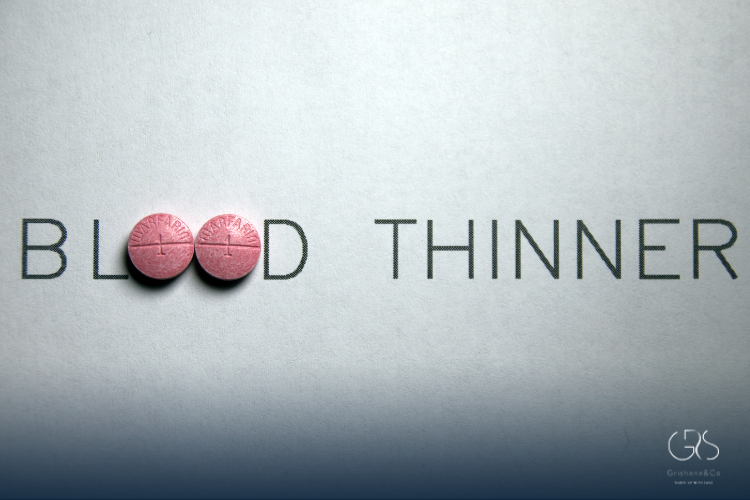
1. Anticoagulant Medications
Heparin: often used in hospitals for short-term prevention.
Warfarin (Coumadin): a vitamin K antagonist that requires INR (International Normalized Ratio) monitoring to maintain therapeutic levels.
Direct Oral Anticoagulants (DOACs): such as apixaban, rivaroxaban, and dabigatran, are increasingly favored for their stable dosing and reduced monitoring needs.
These medications prevent clot formation by interfering with the body’s natural clotting cascade. However, they carry a risk of bleeding and must be used under physician supervision.
2. Antiplatelet Agents
For arterial clot prevention (e.g., stroke or myocardial infarction), drugs like aspirin or clopidogrel may be prescribed to inhibit platelet aggregation.
3. Regular Monitoring
Patients on long-term anticoagulation require periodic blood tests to ensure safety and efficacy. Lifestyle modifications should continue alongside medication for optimal results.
Understanding the pharmacological side of how to prevent blood clots ensures a comprehensive, evidence-based approach tailored to individual risk.
How to Prevent Blood Clots in High-Risk Groups
Certain populations face elevated risks due to age, health status, or physiological changes.
1. Elderly Individuals
Aging reduces mobility and vascular elasticity. Encouraging moderate exercise, routine checkups, and compression therapy can help older adults prevent blood clots effectively.
2. Pregnant and Postpartum Women
Pregnancy increases circulating estrogen and compresses pelvic veins, leading to stasis. Preventive measures include staying active, avoiding prolonged sitting, and consulting obstetricians about compression stockings or safe anticoagulant options.
3. Cancer Patients
Cancer increases coagulability due to tumor-related inflammation and chemotherapy effects. Some patients may require low-molecular-weight heparin or DOACs under medical supervision.
4. Individuals with Cardiovascular or Metabolic Conditions
Patients with hypertension, diabetes, or hyperlipidemia should strictly manage their conditions through diet, medication adherence, and regular cardiovascular screening.
By recognizing and managing these risk profiles, healthcare professionals and patients can significantly reduce thrombosis incidence.
When to Seek Immediate Medical Help
Despite preventive efforts, recognizing early symptoms of a blood clot is crucial for survival:
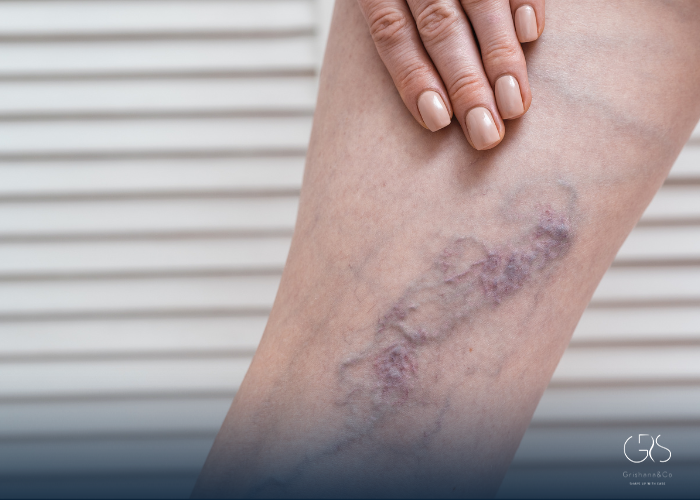
Signs of Deep Vein Thrombosis (DVT):
Swelling in one leg (usually calf or thigh)
Pain, tenderness, or warmth
Skin discoloration (red or bluish tint)
Signs of Pulmonary Embolism (PE):
Sudden shortness of breath
Sharp chest pain or discomfort
Rapid heartbeat or coughing up blood
If any of these symptoms occur, seek emergency medical attention immediately. Prompt treatment can prevent fatal complications.
Conclusion
Preventing blood clots requires a multifaceted approach integrating lifestyle modifications, medical monitoring, and risk awareness. Regular movement, hydration, balanced diet, smoking cessation, and medical guidance are central to vascular health. For those with elevated risks, anticoagulant therapy under supervision can be lifesaving.
Learning how to prevent blood clotsis not just about avoiding disease—it’s about preserving mobility, longevity, and overall well-being through evidence-based, preventive healthcare.
Sources
- Centers for Disease Control and Prevention (CDC), Risk Factors for Blood Clots
- Mayo Clinic, Deep vein thrombosis (DVT)
- World Health Organization (WHO), Physical activity