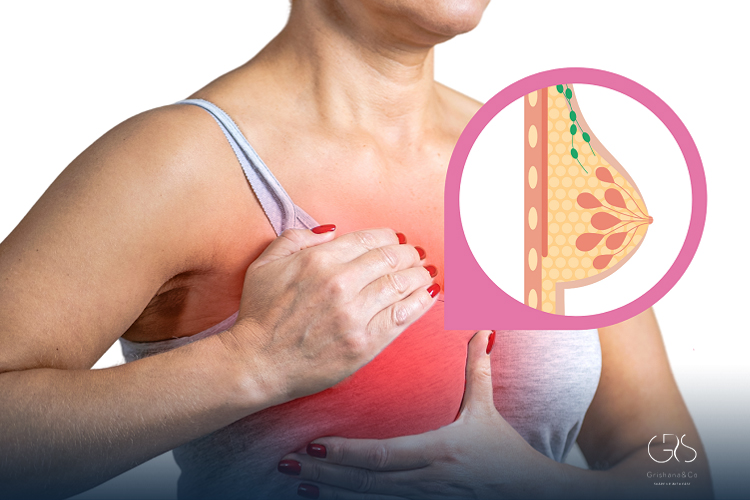
Inflammatory Breast Cancer is a rare but aggressive form of breast cancer that behaves very differently from more common types. Instead of forming a distinct lump, this disease spreads quickly through the skin and lymphatic vessels of the breast, causing visible changes. Because of its unusual presentation, Inflammatory Breast Cancer is often mistaken for an infection or skin condition, which can delay diagnosis. Scientifically, it accounts for only about 1–5% of all breast cancers, yet it causes a disproportionately high number of breast cancer–related deaths due to its rapid progression.
Why Inflammatory Breast Cancer Is Different
Unlike most breast cancers that grow as localized tumors, Inflammatory Breast Cancer spreads diffusely. Cancer cells block lymphatic vessels in the skin, leading to inflammation-like symptoms. This biological behavior explains why redness, swelling, and warmth appear early. Researchers have shown that IBC cells have distinct molecular profiles, including higher rates of HER2 positivity and angiogenesis, which contribute to aggressive growth and early metastasis.

Inflammatory Breast Cancer vs Other Breast Cancers
Traditional breast cancers usually develop slowly and are often detected through screening mammography. In contrast, Inflammatory Breast Cancer often does not show up clearly on routine imaging. Studies indicate that IBC is more likely to be diagnosed at stage III or IV, reflecting how quickly it spreads beyond the breast.
Why It Often Goes Undetected Early
One major challenge is symptom overlap with mastitis or allergic reactions. Antibiotics may be prescribed initially, and when symptoms do not improve, valuable time may have passed. Scientific reviews emphasize the importance of clinical suspicion when breast changes persist beyond one to two weeks.
Common Symptoms You Should Not Ignore
Symptoms of Inflammatory Breast Cancer usually appear suddenly and worsen over days or weeks. Awareness of these signs is critical for early medical evaluation.
Skin Changes and Redness
The breast may appear red, pink, or purplish, covering more than one-third of the breast. This discoloration results from blocked lymph vessels rather than infection.
Swelling and Warmth
Affected breasts often feel warmer and heavier than usual. Research shows that inflammatory signaling molecules released by cancer cells contribute to these sensations.
Pain, Itching, and Texture Changes
Persistent pain, burning, or itching may occur. The skin can thicken and develop a pitted appearance known as peau d’orange, resembling an orange peel.
Nipple Changes
Nipple inversion, flattening, or discharge can happen as the disease affects underlying tissue structures.
Who Is at Higher Risk?
While anyone can develop Inflammatory Breast Cancer, certain factors are associated with increased risk. Epidemiological studies show that IBC is diagnosed at younger ages compared to other breast cancers and is more common in women under 50.
Age and Hormonal Factors
Premenopausal women appear to be affected more frequently. Hormonal influences on breast tissue may partially explain this trend.
Race and Ethnicity
Research consistently shows higher incidence rates among Black women, along with poorer outcomes. Scientists believe this disparity reflects a combination of biological differences, access to care, and systemic healthcare inequities.
Obesity and Metabolic Factors
Higher body mass index has been associated with increased risk. Chronic inflammation linked to obesity may play a role in disease development and progression.
How Inflammatory Breast Cancer Is Diagnosed
Diagnosing Inflammatory Breast Cancer requires a combination of clinical evaluation, imaging, and tissue biopsy. Because symptoms mimic infection, diagnosis relies heavily on physician awareness.
Clinical Examination and Medical History
Doctors assess rapid onset of symptoms and lack of response to antibiotics. Persistent inflammatory signs raise suspicion for Inflammatory Breast Cancer.
Imaging Limitations
Mammography may miss IBC due to the absence of a lump. Ultrasound and MRI are more sensitive in detecting skin thickening and lymphatic involvement.
Biopsy and Pathology
A skin punch biopsy or core needle biopsy confirms the diagnosis. Pathologists look for cancer cells within lymphatic vessels, a hallmark of this disease.
Staging and Spread of the Disease
By definition, Inflammatory Breast Cancer is at least stage III at diagnosis. This staging reflects extensive local involvement.
Local and Regional Spread
Cancer often spreads to nearby lymph nodes early. Studies show high rates of axillary and supraclavicular node involvement at presentation.
Distant Metastasis
Approximately one-third of patients have metastatic disease at diagnosis. Common sites include bone, liver, lung, and brain.
Treatment Approaches Backed by Science
Treatment for Inflammatory Breast Cancer is intensive and multimodal. Decades of clinical trials have shaped current standard care.
Neoadjuvant Chemotherapy
Chemotherapy is typically given first to shrink cancer and control microscopic spread. Anthracycline- and taxane-based regimens are commonly used, supported by large randomized trials.
Targeted and Hormonal Therapies
HER2-positive tumors benefit from targeted drugs such as trastuzumab and pertuzumab, which significantly improve survival. Hormone receptor–positive cases may receive endocrine therapy after initial treatment.
Surgery and Radiation
After chemotherapy, mastectomy with lymph node dissection is standard. Breast-conserving surgery is generally not recommended. Radiation therapy follows surgery to reduce recurrence risk.
Living With and Beyond Diagnosis
A diagnosis of Inflammatory Breast Cancer can feel overwhelming, but advances in treatment have improved outcomes.
Survival Rates and Prognosis
Historically, survival was poor, but modern therapies have increased five-year survival rates to approximately 40–50%. Prognosis depends on stage, tumor biology, and response to therapy.
Emotional and Psychological Impact
Patients often experience anxiety, fear, and grief. Studies emphasize the importance of psychological support and counseling as part of comprehensive care.
Importance of Specialized Care
Outcomes are better when patients are treated at centers experienced with Inflammatory Breast Cancer. Multidisciplinary teams ensure coordinated, evidence-based treatment.
Ongoing Research and Future Directions
Scientific research continues to explore why Inflammatory Breast Cancer behaves so aggressively.
Molecular and Genetic Studies
Researchers are identifying gene expression patterns unique to IBC, including pathways related to inflammation and immune evasion.
Immunotherapy and New Targets
Early clinical trials are investigating immune checkpoint inhibitors and novel targeted agents. These approaches aim to improve survival and reduce toxicity.
Improving Awareness and Early Detection
Public health efforts focus on educating both patients and healthcare providers. Early recognition remains one of the most powerful tools against this disease.
Conclusion
Inflammatory Breast Cancer is a rare but serious condition that demands rapid attention and specialized care. Its unusual symptoms, aggressive nature, and diagnostic challenges make awareness essential. Scientific research has clarified how this disease differs biologically from other breast cancers and has led to more effective treatments. While the journey can be difficult, advances in chemotherapy, targeted therapy, surgery, and radiation have significantly improved outcomes. Understanding the signs, risks, and evidence-based treatments empowers patients and supports earlier diagnosis, which remains crucial for improving survival.
Sources
- National Institutes of Health, Inflammatory Breast Cancer
- Springer Nature, Updates in the Management of Inflammatory Breast Cancer
- Inflammatory Breast Cancer,