A prostate biopsy is a medical procedure used to remove small samples of tissue from the prostate gland so they can be examined under a microscope. The primary goal is to determine whether prostate cancer or other abnormal conditions are present. While the word “biopsy” can sound intimidating, this test is one of the most reliable ways doctors can confirm or rule out cancer and guide appropriate treatment decisions. Many men undergo this procedure every year, and advances in medical technology have made it safer, more accurate, and more tolerable than in the past.
Why Doctors Recommend a Prostate Biopsy
Doctors usually recommend a prostate biopsy when other tests suggest something abnormal. These tests do not diagnose cancer on their own but raise enough concern that tissue confirmation is needed.
Elevated PSA Levels and Prostate Biopsy
The prostate-specific antigen (PSA) blood test measures a protein produced by prostate cells. Higher-than-normal PSA levels can be associated with prostate cancer, but they can also rise due to benign prostatic hyperplasia, prostatitis, recent ejaculation, or even cycling. When PSA levels are persistently elevated or rising rapidly, a prostate biopsy may be advised to determine the underlying cause.
Abnormal Digital Rectal Exam Findings
During a digital rectal exam, a clinician feels the prostate through the rectum to assess its size, shape, and texture. Hard areas, asymmetry, or nodules can be warning signs. An abnormal exam alone does not confirm cancer, but combined with PSA findings, it often leads to recommending a biopsy for clarity.
Types of Prostate Biopsy Techniques
There are several methods used to perform a prostate biopsy. The choice depends on available technology, patient anatomy, infection risk, and physician experience.
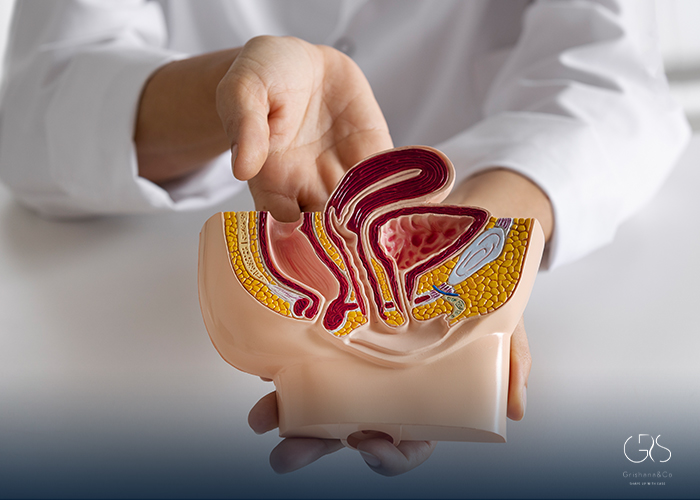
Transrectal Prostate Biopsy Explained
The transrectal approach is the most commonly used technique worldwide. A thin ultrasound probe is inserted into the rectum to visualize the prostate, and a needle is passed through the rectal wall to collect tissue samples. Typically, 10 to 12 cores are taken from different areas to improve detection accuracy.
Transperineal Prostate Biopsy Approach
In the transperineal method, needles are inserted through the skin between the scrotum and anus. This technique significantly reduces the risk of infection because it avoids passing through the rectum. Recent studies show transperineal biopsies may have similar or better cancer detection rates with fewer infectious complications, making them increasingly popular.
How a Prostate Biopsy Is Performed
Understanding what happens during a prostate biopsy can help reduce anxiety and set realistic expectations.
Preparation Before the Procedure
Before the biopsy, patients may be asked to stop blood-thinning medications temporarily to reduce bleeding risk. Antibiotics are commonly prescribed beforehand to prevent infection. Some clinicians also recommend an enema to clear the rectum, especially for transrectal procedures.
Step-by-Step Procedure Experience
The procedure usually takes 10 to 20 minutes and is often done on an outpatient basis. Local anesthesia is applied to minimize discomfort. During sampling, patients may feel pressure or brief snapping sensations as tissue cores are collected. While uncomfortable, the procedure is generally well tolerated, and most men can go home shortly afterward.
Pain, Discomfort, and Recovery Expectations
Pain levels during a prostate biopsy vary from person to person. Most describe the sensation as mild to moderate discomfort rather than severe pain.
Managing Pain During Prostate Biopsy
Local anesthetics, such as lidocaine nerve blocks, significantly reduce pain. Some centers also offer mild sedation for anxious patients. Research shows that adequate anesthesia improves patient comfort without affecting biopsy accuracy.
Recovery Timeline and Aftercare
Recovery is usually quick. Light bleeding in urine, stool, or semen is common for several days to weeks and typically resolves on its own. Patients are advised to avoid strenuous activity for 24 to 48 hours and to stay hydrated. Fever, severe pain, or difficulty urinating should be reported immediately, as these may indicate complications.
Understanding Prostate Biopsy Results
Waiting for biopsy results can be stressful, but understanding the report helps patients make informed decisions.
What the Gleason Score Means
Pathologists grade prostate cancer using the Gleason scoring system, which evaluates how abnormal the cancer cells look. Scores range from 6 to 10, with higher numbers indicating more aggressive disease. This score plays a central role in determining treatment options and prognosis.
Benign and Inflammatory Findings
Not all biopsies reveal cancer. Many show benign prostatic tissue, inflammation, or precancerous changes like prostatic intraepithelial neoplasia. These findings may still require monitoring but do not always mean immediate treatment is necessary.
Accuracy and Limitations of Prostate Biopsy
Although a prostate biopsy is considered the diagnostic gold standard, it is not perfect.
False Negatives and Sampling Error
Because only small tissue samples are taken, cancer can occasionally be missed, especially if it is small or located in hard-to-reach areas. Studies estimate false-negative rates of up to 20%. Repeat biopsy or advanced imaging may be recommended if suspicion remains high.
Role of MRI in Improving Accuracy
Multiparametric MRI has transformed how biopsies are performed. MRI-targeted biopsies allow doctors to focus on suspicious areas rather than sampling randomly. Evidence shows that combining MRI with biopsy improves detection of clinically significant cancers while reducing unnecessary diagnoses.
Risks and Complications to Be Aware Of
Like any medical procedure, a prostate biopsy carries some risks, though serious complications are uncommon.
Infection and Bleeding Risks
Minor bleeding is expected, but severe bleeding is rare. Infection risk is higher with transrectal biopsies due to rectal bacteria, though antibiotic prophylaxis has reduced this significantly. Transperineal approaches further lower infection rates, according to large clinical studies.
Urinary Retention and Rare Complications
Temporary difficulty urinating can occur due to swelling or blood clots, but it usually resolves. Hospitalization after biopsy is uncommon, occurring in less than 5% of patients in most modern studies.
Life After a Prostate Biopsy
After a prostate biopsy, follow-up depends on the results and individual risk factors.
Follow-Up After Normal Results
If results are benign, doctors may recommend continued PSA monitoring and repeat imaging rather than immediate re-biopsy. Lifestyle factors and prostate health may also be discussed to reduce inflammation and improve overall well-being.
Next Steps If Cancer Is Found
If cancer is detected, treatment options range from active surveillance for low-risk disease to surgery, radiation, or systemic therapies for higher-risk cases. Decisions are based on biopsy findings, PSA levels, imaging results, age, and patient preferences.
Conclusion
A prostate biopsy is a critical diagnostic tool that helps clarify whether prostate cancer or other abnormalities are present. While the idea of a biopsy can feel overwhelming, understanding why it’s done, how it works, and what the results mean can make the experience far less intimidating. Advances in imaging, biopsy techniques, and pain management have made the procedure safer and more accurate than ever. Most importantly, the information gained from a biopsy empowers patients and doctors to make informed, personalized decisions about prostate health and long-term care.
Sources
- National Cancer Institute, Prostate Cancer—Patient Version
- European Association of Urology, Prostate Cancer
- Springer Nature, Comparing the biopsy strategies of prostate cancer: a systematic review and network meta-analysis
- JAMA Network, Magnetic Resonance Imaging, Clinical, and Biopsy Findings in Suspected Prostate Cancer