Type 1 diabetes is a chronic condition that requires timely diagnosis and proper management for optimal health outcomes. Diagnosing type 1 diabetes involves a thorough evaluation of symptoms, physical examination, and specific tests. In this article, we will explore the diagnostic process, available tests, relevant statistics, and diverse perspectives on diagnosing type 1 diabetes.
Understanding Type 1 Diabetes
Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is an autoimmune disorder that affects the body’s ability to produce insulin. According to the Centers for Disease Control and Prevention (CDC), approximately 1.6 million Americans have type 1 diabetes. This chronic condition typically develops in childhood or adolescence but can occur at any age.
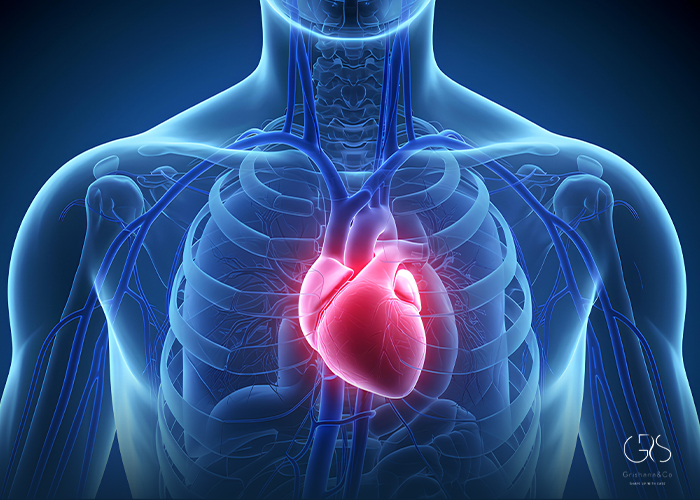
In type 1 diabetes, the body’s immune system mistakenly attacks the insulin-producing cells in the pancreas, leading to a lack of insulin. Insulin is essential for regulating blood glucose levels and allowing cells to utilize glucose for energy. Without sufficient insulin, blood glucose levels rise, leading to hyperglycemia.
Diagnosing Type 1 Diabetes
The process of diagnosing type 1 diabetes involves several key steps:
Medical History and Physical Examination: Healthcare professionals begin the diagnosis by collecting a comprehensive medical history and performing a thorough physical examination. They assess symptoms such as frequent urination, excessive thirst, unexplained weight loss, and fatigue. They also consider risk factors such as family history of type 1 diabetes, age, and ethnicity.

Blood Tests: Blood tests play a crucial role in diagnosing type 1 diabetes. The primary tests used are:a. A1C Test: The A1C test measures a person’s average blood glucose levels over the past two to three months. This test determines the percentage of hemoglobin that has glucose attached to it. An A1C level of 6.5% or higher, confirmed by repeat testing, indicates diabetes.b. Fasting Plasma Glucose (FPG)
Test: This test measures blood glucose levels after fasting for at least eight hours. A fasting blood glucose level of 126 mg/dL or higher on two separate occasions confirms the diagnosis of diabetes.c. Random Plasma Glucose
Test: In this test, blood glucose levels are measured at any time of the day, regardless of the time since the last meal. A random blood glucose level of 200 mg/dL or higher, along with the presence of typical symptoms, indicates diabetes.
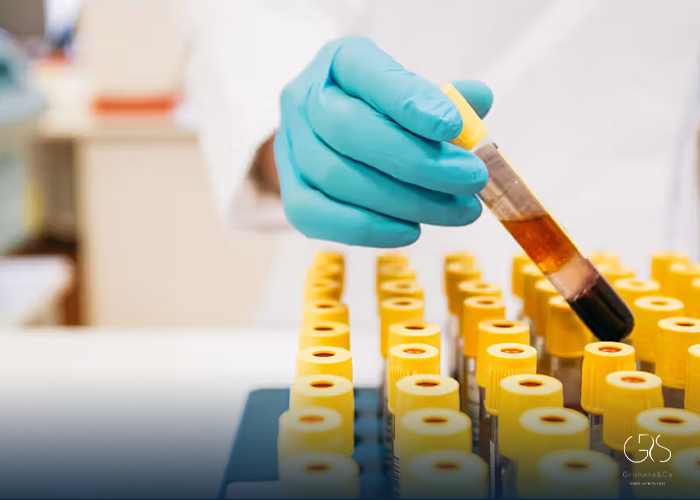
Other Tests: In some cases, additional tests may be necessary to confirm the diagnosis or determine the type of diabetes. These tests may include a glucose tolerance test, islet cell antibodies test, or c-peptide test.
Statistics on Type 1 Diabetes Diagnosis
Understanding the prevalence and incidence of type 1 diabetes is essential to grasp the significance of accurate and timely diagnosis. Here are some relevant statistics:
- Type 1 diabetes accounts for about 5-10% of all diagnosed cases of diabetes in the United States.
- Approximately 40,000 people in the United States receive a type 1 diabetes diagnosis each year.
Diverse Perspectives on Diagnosing Type 1 Diabetes
The process of diagnosing type 1 diabetes involves diverse perspectives from healthcare professionals, researchers, and individuals living with the condition. Various factors can influence the diagnostic process and individual experiences. Let’s explore some of these perspectives:
Age and Diagnostic Challenges: Diagnosing type 1 diabetes in infants, young children, or older adults can present unique challenges. Healthcare professionals need to consider age-related symptoms and potential variations in disease progression.
Symptoms and Misdiagnosis: The symptoms of type 1 diabetes can be similar to other conditions, leading to potential misdiagnosis. It is crucial for healthcare professionals to consider a wide range of symptoms and risk factors while evaluating patients.
Psychological Impact: Receiving a type 1 diabetes diagnosis can have a significant psychological impact on individuals. Anxiety, fear, and a sense of loss may arise. Providing emotional support alongside the diagnosis is essential for well-rounded care.
Treatment Options and Next Steps
Once a diagnosis of type 1 diabetes is confirmed, individuals require immediate treatment to manage their condition effectively. Treatment options typically include:
Insulin Therapy: People with type 1 diabetes require insulin therapy to replace the insulin their bodies cannot produce. Insulin may be administered through multiple daily injections or an insulin pump.

Blood Glucose Monitoring: Regular blood glucose monitoring is vital for assessing treatment effectiveness and maintaining optimal glucose control. Modern devices, such as continuous glucose monitors, offer real-time data and aid in making informed decisions.
Lifestyle Modifications: A healthy lifestyle, including a balanced diet, regular physical activity, managing stress, and getting quality sleep, is essential for managing type 1 diabetes effectively.
Education and Support: Education on diabetes self-care, including carbohydrate counting, insulin administration, and recognizing and managing hyperglycemia and hypoglycemia, is crucial. Support from healthcare professionals, diabetes educators, and support groups can enhance self-management skills.
Conclusion
Diagnosing type 1 diabetes involves a comprehensive evaluation of symptoms, physical examination, and specific tests. The timely and accurate diagnosis of type 1 diabetes is vital for initiating appropriate treatment, managing blood glucose levels, and maintaining overall health.
By understanding the diagnostic process, being aware of relevant statistics, and considering diverse perspectives, healthcare professionals and individuals can collaborate to ensure timely diagnosis and optimal management of type 1 diabetes.
Sources
- Centers for Disease Control and Prevention (CDC), Type 1 Diabetes
- American Diabetes Association (ADA), Diagnosis