If you’ve ever woken up with puffy, itchy eyelids during allergy season, you know how uncomfortable and frustrating it can be. Allergy swollen eyes are one of the most common symptoms of allergic reactions, yet they’re often misunderstood or mistreated. Many people try quick fixes without realizing that effective relief depends on understanding what’s happening inside the body. In this article, we’ll walk through scientifically supported treatment options, explain why swelling happens, and help you choose solutions that actually work.
Understanding Allergy Swollen Eyes
What Causes Allergy Swollen Eyes
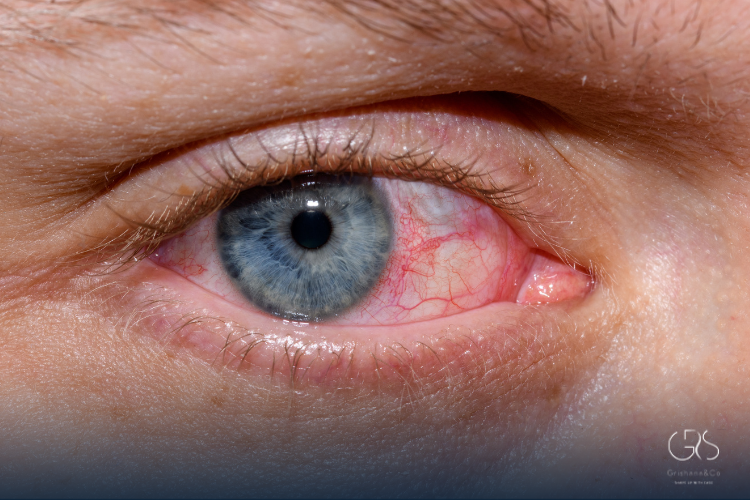
Allergy swollen eyes occur when your immune system overreacts to harmless substances like pollen, dust mites, pet dander, or mold. When allergens come into contact with the eyes, immune cells release histamine and other inflammatory chemicals. These substances increase blood vessel permeability, allowing fluid to leak into surrounding tissues, especially the thin skin around the eyes.
Why the Eye Area Swells So Easily
The skin around the eyes is among the thinnest on the body and contains loose connective tissue. This makes it particularly vulnerable to fluid accumulation. Even mild inflammation can lead to noticeable puffiness, redness, and discomfort compared to other facial areas.
The Role of Histamine in Eye Swelling
How Histamine Triggers Inflammation
Histamine is a key chemical mediator released during allergic reactions. In the eyes, it causes blood vessels to dilate and become leaky, leading to swelling, itching, and tearing. Research shows that blocking histamine receptors significantly reduces allergic eye symptoms, which is why antihistamines are a cornerstone of treatment.
Why Controlling Histamine Matters
Without proper histamine control, allergy swollen eyes can persist for days or weeks, especially during prolonged allergen exposure. Managing histamine doesn’t just reduce swelling; it also prevents secondary issues like eye rubbing, which can worsen inflammation.
Medical Treatments for Allergy Swollen Eyes
Antihistamine Eye Drops
Antihistamine eye drops are among the most effective first-line treatments. These drops directly block histamine receptors in the eye, providing targeted relief. Clinical trials show that topical antihistamines reduce itching and swelling within minutes and are more effective than oral medications for eye-specific symptoms.
Oral Antihistamines
Oral antihistamines work systemically and can help when eye symptoms are part of a broader allergic response, such as hay fever. However, studies indicate they may be less effective for eye swelling alone and can sometimes cause dryness, which may irritate the eyes further.
Mast Cell Stabilizers
Mast cell stabilizers prevent immune cells from releasing histamine in the first place. These medications are most effective when used preventively, especially before allergy season begins. Scientific reviews confirm their role in reducing the frequency and severity of allergy swollen eyes over time.
Corticosteroids: When Are They Needed?
Short-Term Steroid Eye Drops
In severe cases, ophthalmologists may prescribe low-dose corticosteroid eye drops. These reduce inflammation at a cellular level and are highly effective for stubborn swelling. Due to potential side effects like increased eye pressure, studies emphasize short-term use under medical supervision only.
Risks and Safety Considerations
Long-term steroid use is linked to glaucoma and cataract formation. Research strongly supports reserving steroids for short courses when other treatments fail, highlighting the importance of proper diagnosis and follow-up.
Non-Medication Treatments Backed by Science
Cold Compress Therapy
Cold compresses constrict blood vessels and reduce fluid leakage. Clinical evidence shows that applying a cold compress for 10–15 minutes can significantly reduce puffiness and discomfort in allergy swollen eyes. This method is safe, inexpensive, and effective as supportive therapy.

Saline Eye Rinses
Rinsing the eyes with sterile saline helps flush out allergens and inflammatory mediators. Studies demonstrate that regular saline use reduces symptom severity, especially in people exposed to high pollen levels or air pollution.
Lifestyle and Environmental Control Strategies
Reducing Allergen Exposure Indoors
Limiting indoor allergens is a crucial part of managing eye allergies. Scientific studies show that using HEPA air filters, washing bedding in hot water, and keeping windows closed during high pollen counts significantly reduces allergic symptoms.
Personal Habits That Protect the Eyes
Avoiding eye rubbing is essential. Research confirms that rubbing increases histamine release and worsens swelling. Washing hands frequently and changing clothes after outdoor exposure also helps minimize allergen transfer to the eyes.
Nutrition and Immune Support
Anti-Inflammatory Nutrients
Certain nutrients play a role in reducing allergic inflammation. Omega-3 fatty acids have been shown in clinical studies to lower inflammatory markers associated with allergic eye disease. Vitamin C also acts as a natural antihistamine, helping reduce swelling intensity.
Hydration and Eye Health
Proper hydration helps regulate fluid balance in the body. While hydration alone won’t cure allergy swollen eyes, studies suggest it can prevent excessive fluid retention that worsens puffiness around the eyes.
When to See a Doctor
Signs Your Symptoms Need Medical Attention
If swelling is severe, painful, or accompanied by vision changes, medical evaluation is essential. Persistent unilateral swelling may indicate infection or other non-allergic conditions that require different treatment approaches.
Getting the Right Diagnosis
An accurate diagnosis ensures effective treatment. Allergy testing and ophthalmologic exams help distinguish allergy swollen eyes from conditions like blepharitis or conjunctivitis, which require different management strategies.
Long-Term Prevention Strategies
Immunotherapy for Eye Allergies
Allergen immunotherapy, including allergy shots or sublingual tablets, works by retraining the immune system. Long-term studies show that immunotherapy significantly reduces eye symptoms and medication reliance over time.
Building a Sustainable Allergy Plan
Managing allergies is about consistency. Combining environmental control, preventive medication, and healthy habits offers the best long-term outcomes according to clinical guidelines.
Conclusion
Allergy swollen eyes may seem like a minor inconvenience, but they can significantly affect comfort, appearance, and quality of life. Science shows that the most effective treatment combines targeted medications, supportive non-drug therapies, and smart lifestyle adjustments. By understanding the underlying immune response and choosing evidence-based options, you can reduce swelling, protect your eyes, and regain daily comfort. If symptoms persist or worsen, professional guidance ensures safe and effective care tailored to your needs.
Sources
- Cochrane, Topical antihistamines and mast cell stabilisers for treating seasonal and perennial allergic conjunctivitis
- EAACI (European Academy of Allergy & Clinical Immunology), Guidelines on Allergen Immunotherapy: Allergic Rhinoconjunctivitis
- MDPI, phthalmic Formulations for the Treatment of Allergic Conjunctivitis (systematic review)










