Women heart attack symptoms are often subtle and frequently go unrecognized, even though heart disease remains the leading cause of death among women globally. Unlike the dramatic, chest-clutching pain commonly shown in media, a women heart attack may present with less obvious signs—making it harder to detect and leading to dangerous delays in diagnosis and treatment.
According to the American Heart Association and numerous peer-reviewed studies, women are more likely than men to experience so-called “atypical” heart attack symptoms. These symptoms are easily overlooked or attributed to less serious conditions, leading to dangerous delays in diagnosis and treatment.
This article will explore seven heart attack symptoms that women commonly experience—but often ignore. It will also delve into the science behind why symptoms differ in women, the role of risk factors, and what to do if you notice these warning signs.
Why Heart Attack Symptoms Differ in Women
Before we dive into the symptoms, it’s essential to understand why men and women often experience heart attacks differently.
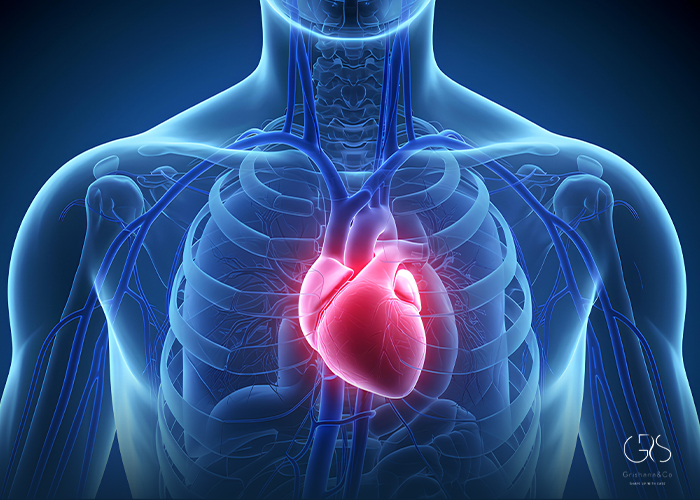
1. Anatomical and physiological differences
Women typically have smaller coronary arteries than men, which means blockages can occur in smaller vessels and still cause serious issues, even if major arteries appear clear. In addition, microvascular dysfunction—a condition affecting the small blood vessels in the heart—is more common in women and can cause heart attack-like symptoms without major artery blockages.
2. Hormonal influence
Estrogen provides some protection to premenopausal women by improving the flexibility of blood vessels and enhancing the lipid profile. However, after menopause, estrogen levels drop, increasing cardiovascular risk and making symptoms more prominent yet harder to distinguish from other age-related changes.
3. Atypical presentation
Women are more likely to show non-classic signs of heart disease, such as fatigue, indigestion, or shortness of breath—symptoms that are often overlooked and not immediately recognized as indicators of a heart problem.
The 7 Overlooked Heart Attack Symptoms in Women
1. Unusual Fatigue
One of the most commonly reported—but easily dismissed—symptoms in women is unusual fatigue. This isn’t just regular tiredness from a busy day. It’s often described as:
- A sudden and unexplained sense of exhaustion
- Fatigue that is overwhelming and persistent, even after rest
- Feeling too weak to do routine activities like walking or talking
Scientific basis: A study published in Circulation (2003) found that 70% of women reported fatigue as a symptom in the days or weeks leading up to a heart attack. Researchers believe this could result from decreased oxygen delivery to tissues due to reduced cardiac output.

2. Shortness of Breath
Many women report difficulty breathing—either at rest or with mild exertion—without chest pain. This symptom can occur:
- During physical activity
- While lying down (orthopnea)
- As a sudden episode without any clear cause
Scientific basis: Shortness of breath is a sign that the heart is struggling to pump efficiently. This leads to a backlog of blood in the pulmonary veins, causing fluid leakage into the lungs, a condition known as pulmonary congestion.
3. Indigestion, Nausea, or Vomiting
Heart attack symptoms in women can mimic gastrointestinal distress. Many women report:
- A burning sensation similar to acid reflux
- Nausea or vomiting
- Bloating or a feeling of fullness, even after small meals
Scientific basis: The vagus nerve, which innervates both the heart and digestive tract, may misinterpret cardiac distress signals as gastrointestinal discomfort. This phenomenon is referred to as visceral cross-talk and can mask the true cardiac origin of symptoms.
4. Pain in the Neck, Jaw, Shoulder, or Upper Back
Instead of the classic left-arm or chest pain, many women experience referred pain to other areas of the body, especially:
- The jaw or throat
- The back between the shoulder blades
- One or both shoulders
Scientific basis: This pattern results from the way sensory nerves transmit pain signals from the heart. In women, pain pathways may be more widely distributed, leading to atypical locations of discomfort.

5. Chest Discomfort (Not Always Severe or Crushing)
While chest pain is the hallmark of heart attacks, women’s experiences often differ. Instead of a crushing or stabbing pain, women describe:
- A feeling of tightness or pressure
- Aching or fullness in the center of the chest
- Pain that comes and goes
Scientific basis: According to data from the Women’s Ischemia Syndrome Evaluation (WISE) study, women are more likely to experience angina equivalents, meaning symptoms that indicate insufficient oxygen to the heart without presenting as classic chest pain.
6. Dizziness or Lightheadedness
Feeling faint, dizzy, or unsteady can be another overlooked sign of a heart attack. This may be accompanied by cold sweats or even a brief loss of consciousness (syncope).
Scientific basis: Poor cardiac output reduces blood flow to the brain. Additionally, arrhythmias or blockages can cause sudden drops in blood pressure, leading to lightheadedness. These symptoms may be mistaken for anxiety or dehydration.
7. Sleep Disturbances
Insomnia or trouble staying asleep, especially if it’s a new issue, can be a subtle warning sign. Many women report:
- Waking frequently during the night
- Trouble falling asleep
- Feeling anxious or restless at night
Scientific basis: The Nurses’ Health Study found that sleep disturbances were linked to increased cardiovascular risk in women. One theory suggests that autonomic nervous system imbalance caused by cardiovascular dysfunction affects sleep regulation.

Risk Factors That Increase the Likelihood of These Symptoms
These symptoms, especially when appearing in combination or suddenly, may indicate a heart attack. However, their likelihood increases if a woman has underlying risk factors, including:
- Diabetes: Women with diabetes are more likely to have silent or atypical heart attacks.
- Hypertension: High blood pressure damages arterial walls and accelerates atherosclerosis.
- Smoking: Strongly associated with early-onset heart disease, especially in women under 55.
- High cholesterol levels
- Obesity or metabolic syndrome
- Family history of heart disease
- Autoimmune disorders (e.g., lupus or rheumatoid arthritis)
- Depression and chronic stress
Notably, emotional stress and mental health issues affect women’s heart health more significantly than men’s. Chronic stress increases cortisol levels, leading to inflammation and endothelial dysfunction.
( If you’re interested in reading about managing high cholesterol)
Why These Symptoms Are Often Ignored
There are several reasons why women and even healthcare providers might dismiss these symptoms:
- Lack of awareness: Media and educational campaigns have historically focused on men’s symptoms.
- Gender bias in medicine: Women’s symptoms are more likely to be attributed to anxiety, stress, or hormonal issues.
- Normalization: Many women attribute fatigue or discomfort to daily stressors, caregiving responsibilities, or menopause.
- Delayed presentation: Women are more likely to wait before seeking medical attention, often dismissing symptoms until they worsen.
A study published in the Journal of the American Medical Association (JAMA) found that women are more likely to die after a heart attack than men, in part because of these diagnostic and treatment delays.
When to Seek Help
If you are experiencing one or more of these symptoms—especially in combination—and you have risk factors for heart disease, do not delay seeking medical attention.
Call emergency services immediately if you notice:
- Chest discomfort lasting more than a few minutes
- Sudden shortness of breath with fatigue or pain
- Jaw or upper back pain without explanation
- Nausea, sweating, and dizziness
Time is muscle. The faster a heart attack is diagnosed and treated, the better the outcome.
Diagnosis and Testing
If you present with any of these symptoms, your doctor may order:
- Electrocardiogram (ECG): Measures electrical activity of the heart.
- Troponin blood test: Detects heart muscle damage.
- Echocardiogram: Visualizes heart movement and function.
- Coronary angiography: Checks for blockages in coronary arteries.
In women, additional tests like stress echocardiography or cardiac MRI may be needed to detect microvascular disease or other atypical presentations.
Prevention: How Women Can Reduce Their Risk
While genetics play a role, lifestyle and preventive care significantly influence heart health.
Key preventive strategies include:
- Quitting smoking protects your heart and lungs
- Eat a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins
- Exercise regularly, aiming for at least 150 minutes per week
- Manage stress through yoga, meditation, or therapy
- Get regular screenings for blood pressure, cholesterol, and diabetes
- Sleep 7–9 hours per night
- Know your family history
Women over 40 should consider discussing their heart health with a cardiologist, especially if they have multiple risk factors or a history of complications like gestational diabetes or preeclampsia.
(If you’re interested in reading about heart-healthy habits)
(To learn more about Sleep Duration please refer to this article)
Conclusion
Heart attacks in women can be silent killers—not because they’re truly silent, but because the symptoms speak a different language. Recognizing these warning signs early can save lives.
By understanding the 7 commonly ignored symptoms—fatigue, shortness of breath, indigestion, referred pain, mild chest discomfort, dizziness, and sleep disturbances—women can advocate more effectively for their health. Greater awareness, combined with appropriate medical care and lifestyle changes, offers the best defense against heart disease.
Sources
- American Heart Association, Warning Signs of a Heart Attack
- CDC, Heart Disease Facts
- National Library of Medicine, Sleep Duration and Risk for Hypertension in Women: Results from The Nurses’ Health Study