Feeling hungry is one of the most basic signals the human body sends, yet there are many times when hunger unexpectedly fades. This experience, known as loss of appetite, can be temporary or persistent, mild or concerning. Although it is sometimes triggered by simple lifestyle changes, it can also be linked to deeper biological, emotional, or medical factors. Understanding why your appetite decreases helps you interpret what your body is trying to communicate and ensures you respond in a healthy and informed way.
Hunger is not just a feeling; it is a biologically coordinated process. Your brain, digestive system, hormones, and sensory perceptions work together to determine when you need food. When any part of this system becomes disrupted, hunger cues may weaken or disappear altogether. This article explores the scientific mechanisms behind appetite changes, helping you understand why you may not feel hungry and what steps can support appetite recovery.
How the Body Regulates Hunger and Why Loss of Appetite Happens
Hunger regulation begins in the brain, specifically in the hypothalamus, which receives signals about the body’s energy needs. Hormones such as ghrelin, leptin, insulin, and cortisol play essential roles in controlling appetite. Ghrelin triggers hunger, while leptin signals fullness. Insulin helps balance blood sugar, and cortisol affects hunger responses during stress. When these signals become unbalanced due to illness, hormonal changes, emotional strain, or inflammation the result may be loss of appetite. This natural response is often the body’s way of conserving energy or protecting the digestive system while it focuses on healing or adapting to stress.

Medical Conditions That Contribute to Loss of Appetite
Many medical issues directly influence appetite. Viral infections like influenza or COVID-19 often lead to temporary loss of appetite because the immune system releases inflammatory chemicals that reduce hunger. Digestive disorders such as gastritis, acid reflux, irritable bowel syndrome, and constipation can make eating uncomfortable or cause fullness quickly. Chronic diseases including kidney disease, liver disease, cancer, and heart failure may reduce appetite through metabolic changes or nausea. Hormonal conditions such as hypothyroidism can slow digestion and energy use, reducing hunger. When appetite loss is accompanied by weight loss, fever, pain, or ongoing fatigue, medical evaluation is very important.
Emotional and Psychological Factors Affecting Hunger
Mental and emotional health have a powerful impact on appetite. Stress activates the fight-or-flight response, decreasing digestive activity and weakening hunger cues. Anxiety commonly causes stomach tightness, nausea, or rapid heartbeat, all of which reduce appetite. Depression is strongly associated with appetite changes; in many cases, pleasure responses in the brain diminish, making food unappealing. Traumatic events, grief, burnout, and chronic emotional strain may also cause loss of appetite. Because emotional well-being is so closely connected to hunger, addressing psychological factors is essential when appetite changes appear without a physical cause.

Lifestyle Habits That Influence Appetite
Everyday habits can significantly affect how hungry you feel. Poor sleep disrupts hunger-regulating hormones, often causing reduced appetite during the day. High caffeine consumption can suppress hunger and irritate the stomach. Skipping meals regularly weakens natural hunger cues over time. Intense physical activity sometimes leads to temporary loss of appetite as the body redirects blood flow from digestion to the muscles. Alcohol may interfere with digestion and blood sugar stability, reducing hunger the next day. A busy, fast-paced lifestyle can also cause people to ignore subtle hunger cues, eventually lowering appetite naturally.
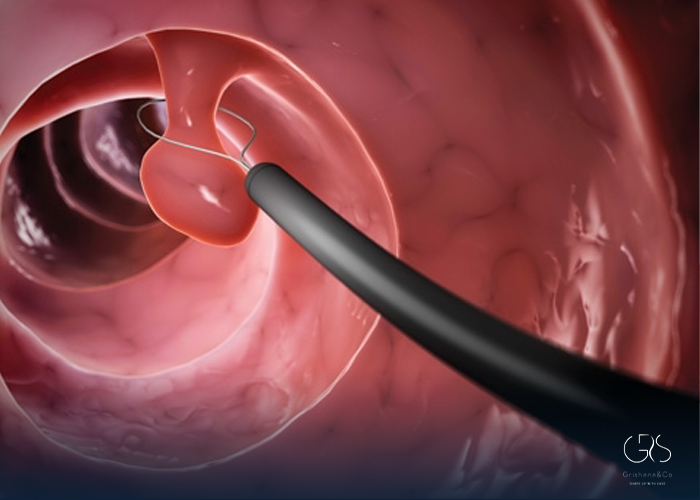
Digestive Problems and Their Effect on Hunger
The digestive system directly influences appetite. If digestion becomes slow or uncomfortable, hunger may decrease. Conditions such as ulcers, gastritis, gastroparesis, and bloating make eating unpleasant, leading to avoidance of food. Food intolerances like lactose or gluten sensitivity can trigger digestive symptoms that decrease appetite over time. Infections in the digestive tract often cause nausea, vomiting, or diarrhea, contributing to short-term loss of appetite. Even mild gut microbiome imbalances can affect appetite because the brain and digestive system communicate closely through hormonal and neurological pathways.
Hormonal Fluctuations and Hunger Changes
Hormones influence metabolism and appetite more than most people realize. Pregnancy often causes nausea and appetite changes due to rapid shifts in hCG and estrogen. Menopause brings significant hormonal transitions that influence appetite, digestion, and energy levels. Thyroid disorders disrupt metabolic speed and can reduce hunger. Chronic stress may raise cortisol levels for long periods, sometimes leading to appetite suppression as the body becomes overwhelmed. Even natural menstrual cycle phases can cause hunger changes, demonstrating how sensitive appetite is to hormonal balance.
Aging and Reduced Hunger in Older Adults
As people age, appetite naturally changes. The senses of taste and smell may become less sharp, making food less appealing. Digestion often slows, leading to longer feelings of fullness. Many older adults take medications that reduce appetite or cause mild nausea. Social factors such as loneliness, reduced physical activity, or lack of routine can also greatly influence meal interest. While occasional low appetite is normal, long-term appetite loss in older adults can lead to nutrient deficiencies and unintentional weight loss, making awareness and monitoring essential.
How Illness and Inflammation Cause Appetite Loss
When the body fights infection, it often reduces appetite intentionally. During illness, inflammatory chemicals called cytokines affect the brain’s hunger centers, reducing interest in food. Fever raises metabolic demands while decreasing hunger. Respiratory infections may affect smell and taste functions, significantly reducing appetite. Gastrointestinal infections disrupt digestion and nearly always cause temporary loss of hunger. These responses help the body focus on recovery, but hydration and gentle nutrition remain important during illness.
Nutritional Deficiencies and Their Impact on Appetite
Certain nutrient deficiencies can cause loss of appetite. Low zinc levels alter taste and smell, making food less satisfying. Vitamin B deficiencies affect energy levels and neurological function, weakening appetite. Iron deficiency can cause fatigue, dizziness, and digestive discomfort, reducing interest in meals. These deficiencies may create a cycle in which appetite continues to drop, even though the body needs more nutrients, making diagnosis and correction essential.
When Loss of Appetite Requires Medical Attention
Most brief appetite changes are not dangerous, but long-lasting or unexplained loss of appetite can become a serious concern. If reduced hunger lasts more than a few days, leads to significant weight loss, affects hydration, causes weakness, or is accompanied by severe emotional distress, a medical evaluation is necessary. Doctors may use blood tests, imaging, medication reviews, and dietary assessments to identify the underlying cause. Early intervention helps prevent nutritional deficiencies and ensures proper treatment for any hidden conditions.
Ways to Support Healthy Appetite Recovery
Supporting appetite recovery involves both physical and emotional strategies. Eating small, nutrient-rich meals helps maintain energy without overwhelming the stomach. Drinking enough water improves digestion and supports appetite signals. Light exercise such as walking stimulates hunger hormones naturally. Improving sleep, reducing stress, and practicing relaxation techniques can restore normal appetite rhythms. Enhancing food flavor, temperature, and texture often makes meals more appealing. If medications affect hunger, adjusting timing or discussing alternatives with a healthcare provider may help. Above all, understanding your body’s patterns helps you respond in a supportive and effective way.
(I recommend that you read about appetite regulation.)
Final Thoughts: Understanding Your Body’s Hunger Signals
loss of appetite is a meaningful signal from your body that something has changed—physically, emotionally, or hormonally. While many causes are temporary and harmless, others require attention to protect long-term health. By understanding how hunger works and recognizing the factors that influence it, you can better interpret changes in appetite and take steps toward restoring balance. Whether the cause is stress, illness, lifestyle habits, or hormonal shifts, awareness empowers you to nourish your body in a healthier and more intentional way.
Sources
- APA, Stress effects on the body
- PubMed Central (PMC), An overview of appetite decline in older people
- National Institute of Diabetes and Digestive and Kidney Diseases, Digestive Diseases