Pregnancy is a beautiful journey that comes with its share of challenges. Unfortunately, some women may experience complications during pregnancy, such as preeclampsia. Preeclampsia is a condition that affects pregnant women and poses significant risks to both the mother and the baby. It is crucial to understand the different types of preeclampsia, its symptoms, causes, risk factors, diagnosis, treatment, prevention, and possible complications to promote early detection and appropriate management.
Types of Preeclampsia:
Preeclampsia can be classified into two main types based on the gestational age at which it occurs:
- Early-Onset Preeclampsia: This type typically develops before the 34th week of pregnancy. It is often associated with severe symptoms and poses a higher risk to both the mother and the baby.
- Late-Onset Preeclampsia: This type occurs after the 34th week of pregnancy. Although potentially less severe, it can still have adverse effects on the mother and the baby.
Symptoms of Preeclampsia:
Preeclampsia may manifest through various symptoms, including:
- High blood pressure (hypertension)
- Swelling in the hands, face, and feet
- Proteinuria (the presence of protein in the urine)
- Severe headaches
- Changes in vision, such as blurred vision or sensitivity to light
- Upper right abdominal pain
- Shortness of breath

Causes of Preeclampsia:
The exact cause of preeclampsia is not yet fully understood. However, several factors are believed to contribute to its development:
- Abnormal placenta development: Issues with the formation of blood vessels in the placenta can lead to inadequate blood supply and subsequently cause preeclampsia.
- Problems with blood vessels: Preeclampsia is often characterized by the narrowing and constriction of blood vessels, reducing blood flow to vital organs and tissues.
- Immune system disorders: An overactive immune response in pregnancy can trigger inflammation and contribute to the development of preeclampsia.
- Genetic factors: Some genetic factors may increase the susceptibility to preeclampsia in certain individuals.
- Pre-existing medical conditions: Women with pre-existing conditions, such as high blood pressure or diabetes, have a higher risk of developing preeclampsia.
Risk Factors for Preeclampsia:
While preeclampsia can affect any pregnant woman, certain factors increase the risk:
- First-time pregnancy: Women experiencing their first pregnancy are at a higher risk of developing preeclampsia.
- Previous history of preeclampsia: Women who have experienced preeclampsia in previous pregnancies are at an increased risk of recurrence.
- Multiple pregnancies: Carrying twins, triplets, or more increases the likelihood of developing preeclampsia.
- Age: Pregnant women under 20 or over 40 years old have a higher risk of preeclampsia.
- Obesity: Being overweight or obese prior to pregnancy is a risk factor for developing preeclampsia.
- Chronic hypertension or kidney disease: Women with pre-existing high blood pressure or kidney disease have an elevated risk of preeclampsia.
- Family history: Having a family history of preeclampsia may increase the likelihood of developing the condition.
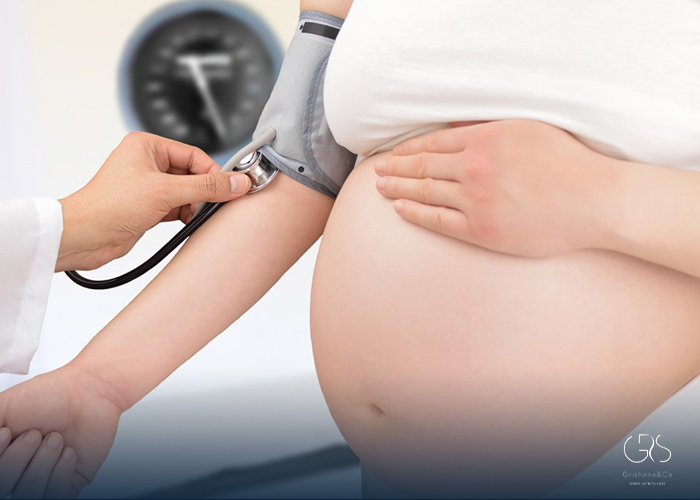
Diagnosis of Preeclampsia:
Early detection and diagnosis of preeclampsia are crucial for effective management. Healthcare providers use the following methods to diagnose preeclampsia:
Blood pressure monitoring: Regularly measuring blood pressure is key in diagnosing preeclampsia. Consistently high readings may indicate the condition.

Proteinuria testing: A urine sample is collected and analyzed to detect the presence of protein. Increased protein levels suggest preeclampsia.
Additional tests: Blood tests may be performed to evaluate liver and kidney function. Ultrasounds can help assess fetal well-being and monitor growth.
Treatment of Preeclampsia:
The treatment of preeclampsia depends on the severity of the condition and the gestational age of the baby.
Treatment options include:
- Medications: Medications to lower blood pressure and prevent seizures (eclampsia) may be prescribed.
- Bed rest and close monitoring: In less severe cases, rest and regular check-ups may be recommended to monitor blood pressure, proteinuria, and other symptoms.
- Corticosteroids: If preterm birth is expected, corticosteroid injections may be given to help with fetal lung development.
- Early delivery: If preeclampsia worsens or poses significant risks to the mother or the baby, early delivery may be necessary for their well-being.
Prevention of Preeclampsia:
Prevention strategies aim to minimize the risk of developing preeclampsia, although they may not guarantee complete prevention.Some measures that may help reduce the risk include:
- Regular prenatal care: Attending regular check-ups and monitoring blood pressure, urine, and other vital signs can aid in early detection.
- Healthy lifestyle: Eating a balanced diet, exercising regularly, and avoiding excessive weight gain during pregnancy are important factors in reducing the risk.
- Treatment of pre-existing conditions: Managing pre-existing medical conditions, such as high blood pressure or diabetes, before pregnancy can reduce the risk of preeclampsia.
Complications Associated with Preeclampsia:
Preeclampsia, if left untreated or poorly managed, can lead to severe complications for both the mother and the baby.Potential complications include:
- Premature birth: Preeclampsia may necessitate the need for early delivery, potentially leading to complications associated with preterm birth.
- Placental abruption: Preeclampsia increases the risk of the placenta detaching from the uterine wall before delivery, which can be life-threatening for both the mother and the baby.
- Organ damage: Preeclampsia can harm vital organs such as the kidneys, liver, and brain, potentially leading to long-term health issues.
- Fetal growth restriction: Insufficient blood supply and nutrients to the baby due to preeclampsia can result in poor fetal growth.
- Stillbirth: In severe cases, preeclampsia may lead to the tragic loss of the baby in the womb.
Conclusion:
Preeclampsia is a serious condition that demands attention and awareness during pregnancy. Understanding the different types, recognizing symptoms, knowing the causes and risk factors, seeking prompt diagnosis and treatment, following preventive measures, and being aware of potential complications can significantly improve the management and outcomes for both the mother and the baby.
Sources
- American Pregnancy Association, Preeclampsia
- Mayo Clinic, Preeclampsia
- National Institute of Child Health and Human Development, Preeclampsia and Eclampsia
- Preeclampsia Foundation, WHAT IS PREECLAMPSIA